Nanobodies against cancer: A wrecking ball against tumour cells?
New research project: Approach offers great potential for personalised cancer medicine
Advertisement
cancer cells often survive even strong therapies, partly due to a protein called survivin. A research team at the Center of Medical Biotechnology at the University of Duisburg-Essen is now looking to disable this protection specifically. The aim is to bind survivin and break it down using novel nanobodies. This could make tumour cells more sensitive to treatment again. The project is funded by the Brigitte and Dr Konstanze Wegener Foundation.
Cancer cells have many strategies for resisting therapy. One such strategy is survivin, a protein that drives the division of diseased cells and prevents them from dying. It is found in large quantities in almost all tumours, but is difficult to target with conventional drugs.
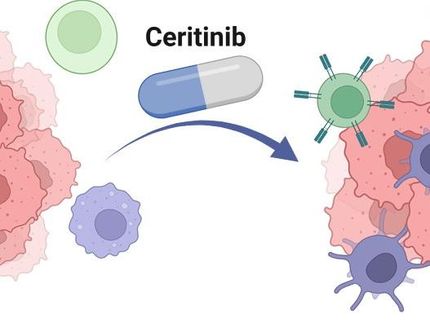
Enter a new project led by Prof. Dr. Shirley Knauer from the Faculty of Biology at the University of Duisburg-Essen: she and her team are developing bespoke small antibody fragments, known as nanobodies, which recognise survivin with great selectivity. Because they are smaller and more stable than conventional antibodies, they can reach structures that are virtually inaccessible to other active substances.
The project combines molecular biology, biochemistry and structural biology approaches. The researchers couple the nanobodies to a degradation signal, prompting the cell’s own machinery to break down survivin – a strategy known as targeted protein degradation using PROTACs (Proteolysis Targeting Chimeras). In simple terms, the nanobody binds to survivin, which causes the protein to lose its function and be directed to an enzyme complex that breaks it down. This causes the cancer cell to lose an important protective mechanism.
The researchers hope that this will make tumours more responsive to conventional therapies and open up new treatment possibilities. In addition, the modular structure of their method means that it could be transferred to other target proteins in the future. “Our approach therefore offers great potential for personalised cancer medicine,” says Knauer. “The funding will enable us to further develop this promising therapeutic platform.”