New starting point discovered in the fight against Pseudomonas aeruginosa
Research team shows how an enzyme regulates the pathogenicity of a clinically relevant pathogen
Advertisement
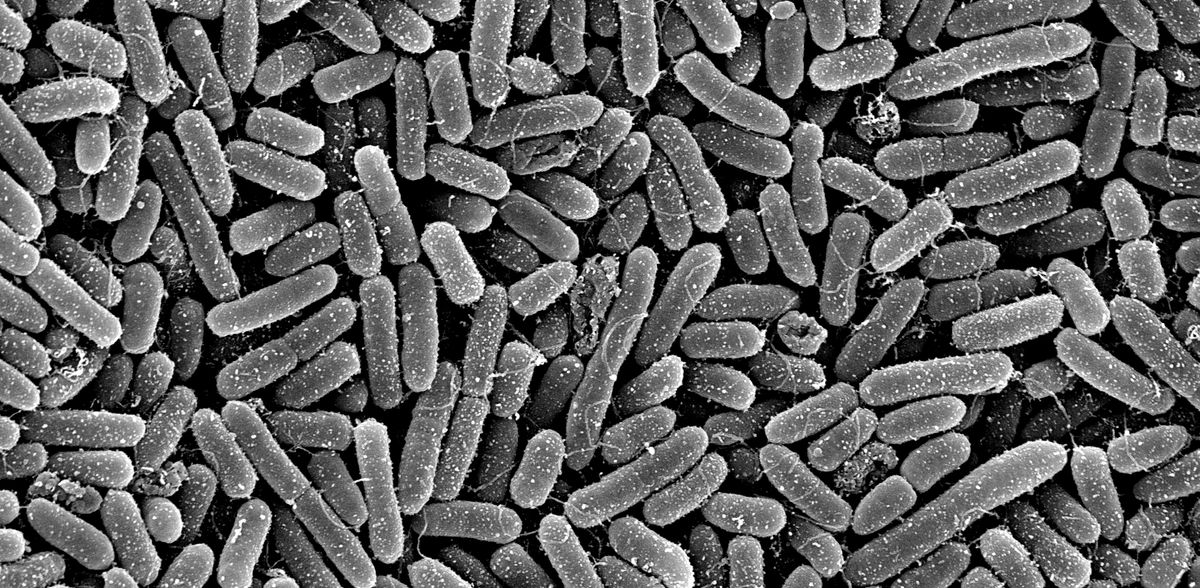
Pseudomonas aeruginosa is an important opportunistic pathogen responsible for life-threatening infections that are associated with high rates of morbidity and mortality. Researchers from TWINCORE, the Centre for Experimental and Clinical Infection Research in Hannover, and the Helmholtz Centre for Infection Research (HZI) in Braunschweig have now been able to show that an enzyme controls virulence through modification of tRNAs. They hope that their findings will pave the way for the development of new treatments. The study has been published in the scientific journal Proceedings of the National Academy of Sciences (PNAS).
Pseudomonas aeruginosa infections can spread via a person to person contact, but they can also arise in various environments. The bacterium thrives in moist conditions, including tap water, dishwashers, sinks, showers or toilets. Moreover, it can be found in soil and water. "The problem is that you can't really avoid Pseudomonas aeruginosa," says Prof Susanne Häußler, Head of the Institute for Molecular Bacteriology at TWINCORE and the department of the same name at the HZI. "In addition, the bacteria can form biofilm communities, which are embedded in a self-produced matrix that protects them from immune cells and antibiotics." In this way, P. aeruginosa is naturally insensitive to a large number of antibiotics and is therefore one of the most problematic hospital germs. Research into the development of so-called pathoblockers, which, unlike antibiotics, do not aim to kill the pathogen but to prevent or weaken its pathogenic effect, is being conducted at full speed.
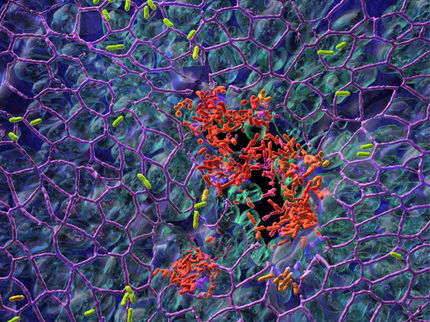
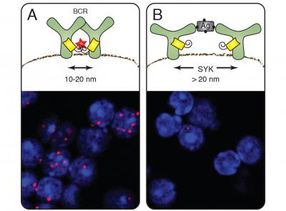
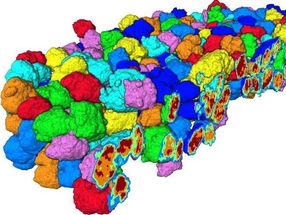
Studies have shown that an enzyme called GidA is significantly involved in communication (quorum sensing) between bacterial cells and the formation of biofilms in P. aeruginosa. Could GidA possibly also be central to the pathogenicity of P. aeruginosa and therefore a potential target for future pathoblockers? Susanne Häußler and her team investigated this question in their current study. GidA is an enzyme which modifies key tRNA molecules. tRNA molecules are involved in protein production through their capacity to decode the genetic code - and GidA gives some of them the finishing touches, so to speak. "We investigated what happens when GidA can no longer make changes to tRNA molecules, and explored the consequences on bacterial pathogenicity," says HZI scientist Dr Nicolas Oswaldo Gomez, one of the first authors of this study. For their investigations, the researchers used genetic methods to produce a bacterial strain of P. aeruginosa that was no longer able to produce the enzyme GidA. In various experimental settings using cell culture and animal models, the researchers compared the pathogenicity of the genetically modified bacteria with that of the wild type. "In all experiments, pathogenicity was significantly reduced compared to the wild type. If GidA is not present, some tRNA molecules are no longer modified, which obviously means that proteins that are crucial for pathogenicity are no longer produced," says Gomez. "In further investigations, for example, we were able to determine that the structure of the biofilm was altered and that a quinolone antibiotic was significantly more effective than in the wild type." Häußler adds: "If tRNA molecules cannot be modified by GidA, Pseudomonas aeruginosa significantly loses its effectiveness and the biofilm protective barrier becomes permeable. These are extremely promising results with regard to new potential targets for the development of pathoblockers!"
Using various OMICS methods and bioinformatic analyses, the researchers were also able to show exactly which types of tRNA molecules are modified by GidA and at which points. And that these modified tRNA molecules only come into play during the synthesis of certain proteins and either at the start or end of genes. "The results of our study make it clear that the pathogenicity of Pseudomonas aeruginosa is subject to a specialised epigenetic control process in which GidA functions like a kind of overriding switch," says Häußler. "And we can and should utilise this - as a starting point for the development of effective pathoblockers against Pseudomonas aeruginosa and other highly problematic bacterial pathogens." In subsequent studies, the researchers want to search for other enzymes that are involved in the modification of tRNA molecules.
In addition to the researchers from TWINCORE and HZI, other cooperation partners from several research institutions were involved in the study, including the Hannover Medical School, the University of Würzburg, and the University of Hamburg.
Original publication
Jonas Krueger, Matthias Preusse, Nicolas Oswaldo Gomez, Yannick Noah Frommeyer, Sebastian Doberenz, Anne Lorenz, Adrian Kordes, Svenja Grobe, Mathias Müsken, Daniel P. Depledge, Sarah L. Svensson, Siegfried Weiss, Volkhard Kaever, Andreas Pich, Cynthia M. Sharma, Zoya Ignatova, Susanne Häussler; "tRNA epitranscriptome determines pathogenicity of the opportunistic pathogen Pseudomonas aeruginosa"; Proceedings of the National Academy of Sciences, Volume 121, 2024-3-7