Gene scissors repair defective immune cells
CRISPR-Cas9 can be used to repair hereditary genetic defects that lead to an excessive immune response, which can be fatal
Advertisement
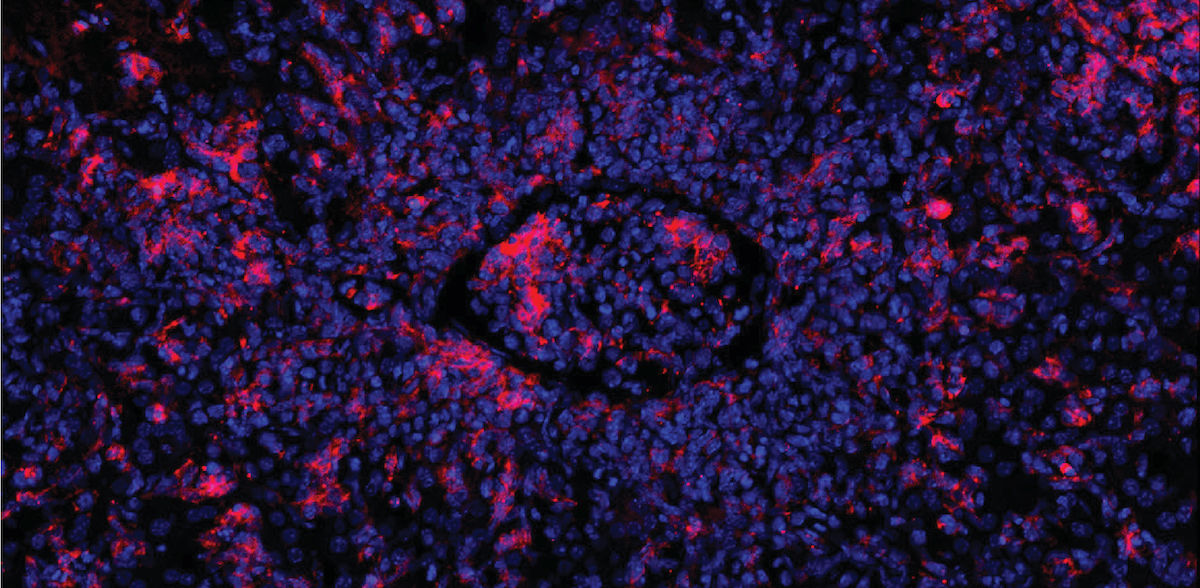
Familial hemophagocytic lymphohistiocytosis (FHL) is a rare disease of the immune system. It usually affects infants and young children up to 18 months of age. The disease is severe and mortality is high. It is caused by various gene mutations that prevent cytotoxic T cells from functioning normally. These are a group of immune cells that kill body cells infected by viruses or otherwise altered. If an affected child becomes infected - for example with the Epstein-Barr virus (EBV), but also with other viruses - the cytotoxic T cells cannot eliminate the infected cells. Instead, the immune response gets out of hand. This leads to a cytokine storm and an excessive inflammatory reaction that affects the entire organism.
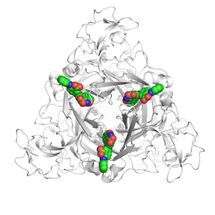
"Doctors combine chemotherapy, immunosuppression and bone marrow transplantation for treatment. Nevertheless, many of the sick children die," says Professor Klaus Rajewsky, head of the "Immune Regulation and Cancer" working group at the Max Delbrück Center. Together with his team, he has developed a new therapeutic principle. The researchers have succeeded in repairing defective T cells from mice and two affected babies using the CRISPR-Cas9 gene scissors. The repaired cytotoxic T cells then functioned normally. The diseased mice recovered from hemophagocytic lymphohistiocytosis.
Repair works in mice
The starting point for the work was mice in which the team was able to simulate EBV infections. In these animals, the researchers altered a gene called perforin in such a way that it lost its function - a common genetic defect in FHL sufferers. If they then triggered a condition similar to an EBV infection, the affected B cells multiplied uncontrollably because the defective cytotoxic T cells were unable to eliminate them. As a result, the immune response went into overdrive and the mice developed hemophagocytic lymphohistiocytosis.
The team then obtained T memory stem cells, i.e. long-lived T cells from which active cytotoxic T cells mature, from the blood of the mice. The researchers used the CRISPR-Cas9 gene scissors to repair the defective perforin gene of the memory T cells and injected them into the animals. The immune response calmed down and the mice recovered from their symptoms.
How long the protective effect lasts is uncertain
The first author of the study, Dr. Xun Li, used blood samples from two sick infants to test whether the principle also works in humans. One of the children had a defective perforin gene, while the second had a different gene affected. "Our gene repair method is more precise than previous approaches and the T cells are almost unchanged after gene repair," says Li. "It was also fascinating to see how effectively the memory T cells could be multiplied and repaired even from a small amount of blood." According to the experiments in cell cultures, the repaired T memory cells of the babies were capable of a normal cytotoxic T cell response.
The active principle therefore works in principle. Before it can benefit patients, the team still needs to clarify open questions and test the treatment concept in clinical trials. "It is still uncertain how long the protective effect will last," says Dr. Christine Kocks, a scientist in Rajewsky's team. "As the T memory stem cells remain in the body for a long time, we hope for long-term or even permanent protection. It is also conceivable that patients could be given their repaired T cells again and again."
Due to the small amount of blood taken, the procedure is gentle and no preparatory treatment was necessary for the mice - unlike a bone marrow transplant, for example, says Rajewsky: "We very much hope that our active principle will be a breakthrough for the treatment of patients with FHL - either to gain time for a successful bone marrow transplant or even as a therapy itself.
Note: This article has been translated using a computer system without human intervention. LUMITOS offers these automatic translations to present a wider range of current news. Since this article has been translated with automatic translation, it is possible that it contains errors in vocabulary, syntax or grammar. The original article in German can be found here.
Original publication
Xun Li, Tristan Wirtz, Timm Weber, Mikhail Lebedin, Elijah D. Lowenstein, Thomas Sommermann, Andreas Zach, Tomoharu Yasuda, Kathrin de la Rosa, Van Trung Chu, Johannes H. Schulte, Ingo Müller, Christine Kocks, Klaus Rajewsky; "Precise CRISPR-Cas9 gene repair in autologous memory T cells to treat familial hemophagocytic lymphohistiocytosis"; Science Immunology, Volume 9