A new treatment strategy against MERS
Licensed drugs effective in cells
Advertisement
First identified in 2012, the MERS-coronavirus is capable of causing severe and often fatal pneumonia. There are no effective treatments for MERS. Researchers from the German Center for Infection Research (DZIF) at Charité – Universitätsmedizin Berlin recently identified a cellular recycling process known as autophagy as a potential target in the fight against MERS. Autophagy-inducing substances – including certain licensed drugs – were shown to be capable of drastically reducing the rate at which the virus replicates.
The MERS pathogen is capable of causing a flu-like illness (Middle East Respiratory Syndrome) which is often associated with pneumonia. Since its appearance in 2012, approximately 2,500 cases have been reported to the WHO across a total of 27 countries. Approximately one third of infections have resulted in death. A team co-led by PD Dr. Marcel Müller of the Institute of Virology on Campus Charité Mitte recently discovered that the MERS virus can only replicate efficiently if it inhibits a cellular process known as autophagy. Based on this initial discovery, the researchers went on to identify substances which are capable of inducing autophagy and can thus be used to limit viral infection.
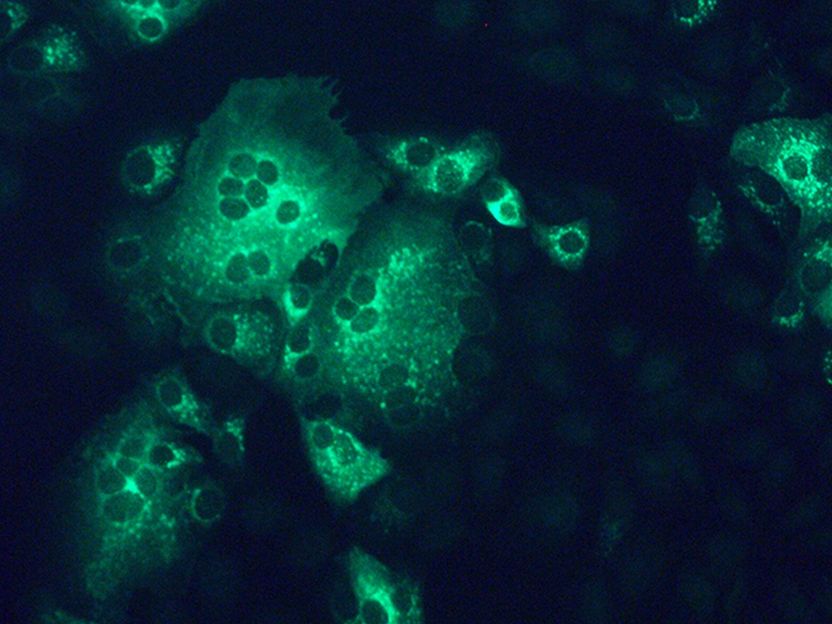
Monkey kidney cells infected with MERS-coronavirus (green). Charité researchers have discovered that the use of SKP2 inhibitors can significantly reduce viral replication.
Müller/Charité
The term autophagy refers to a type of cellular recycling process which enables cells to dispose of damaged materials and waste products, while retaining intact components for incorporation into new cellular structures. This autophagic degradation, or ‘auto-digestion’, is also capable of identifying pathogen-derived components, such as the building blocks of viruses, which are treated as waste products and eliminated. A range of viruses are known to have developed strategies to dysregulate or inhibit autophagy. PD Dr. Müller and his colleagues therefore set out to determine whether the MERS virus is capable of modulating autophagic degradation. As a first step, and using stringent biosafety conditions, the researchers infected cells with the MERS virus. Subsequent observations revealed a disruption to the cellular recycling process in cells infected with the virus. “This result clearly indicated that the MERS pathogen benefits from an attenuation of the cellular recycling process,” explains PD Dr. Müller.
The researchers also succeeded in identifying a previously unknown molecular switch which regulates the process of autophagic degradation: the SKP2 protein. The researchers discovered that the MERS virus activates this molecular switch in order to slow down the cell’s recycling processes and avoid degradation. Using these new insights, the researchers treated MERS-infected cells with various SKP2 inhibitors in order to stimulate the degradation process. This strategy proved successful, the autophagy-inhibiting substances reducing viral replication by a factor of 28,000. Among the substances used to elicit this effect were licensed drugs such as niclosamide, a treatment for tapeworms which had previously been identified as an SKP2 inhibitor. Importantly, niclosamide was shown to be capable of drastically reducing the replication of the MERS virus in cell culture.
“Our results reveal SKP2 to be a promising starting point for the development of new substances capable of fighting the MERS virus, and potentially even other autophagy-dependent viruses,” says PD Dr. Müller. SKP2 inhibitors do not target the virus directly. For this reason, the research group leader expects their use to be associated with a reduced risk of resistance. “However, SKP2 inhibitors will need to be tested in vivo before they can be used as drugs. Furthermore, one has to properly evaluate the risks and benefits for their in vivo use, since even drugs that have already been approved can have side effects,” says the virologist. The researchers will also test whether SKP2 inhibitors could be effective against other coronaviruses such as SARS or the novel coronavirus (2019-nCoV) which is currently emerging in China.