Slipping through cell walls, nanotubes deliver high-potency punch to cancer tumors in mice
Advertisement
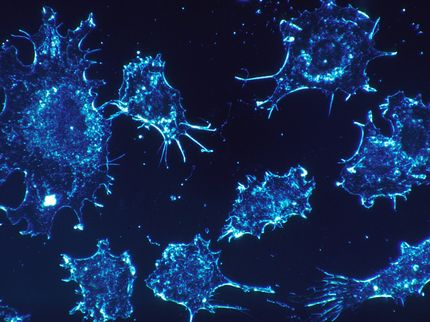
The problem with using a shotgun to kill a housefly is that even if you get the pest, you'll likely do a lot of damage to your home in the process. Hence the value of the more surgical flyswatter. Cancer researchers have long faced a similar situation in chemotherapy: how to get the most medication into the cells of a tumor without "spillover" of the medication adversely affecting the healthy cells in a patient's body.
Now researchers at Stanford University have addressed that problem using single-walled carbon nanotubes as delivery vehicles. The new method has enabled the researchers to get a higher proportion of a given dose of medication into the tumor cells than is possible with the "free" drug - that is, the one not bound to nanotubes - thus reducing the amount of medication that they need to inject into a subject to achieve the desired therapeutic effect.
"That means you will also have less drug reaching the normal tissue," said Hongjie Dai, professor of chemistry and senior author of a paper in Cancer Research. So not only is the medication more effective against the tumor, ounce for ounce, but it greatly reduces the side effects of the medication.
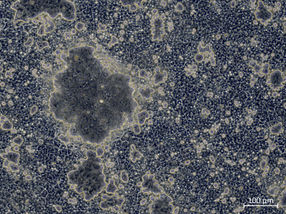
Dai and his colleagues worked with paclitaxel, a widely used cancer chemotherapy drug, which they employed against tumors cells of a type of breast cancer that were implanted under the skin of mice. They found that they were able to get up to 10 times as much medication into the tumor cells via the nanotubes as when the standard formulation of the drug, called Taxol®, was injected into the mice.
The tumor cells were allowed to proliferate for about two weeks prior to being treated. After 22 days of treatment, tumors in the mice treated with the paclitaxel-bearing nanotubes were on average less than half the size of those in mice treated with Taxol.
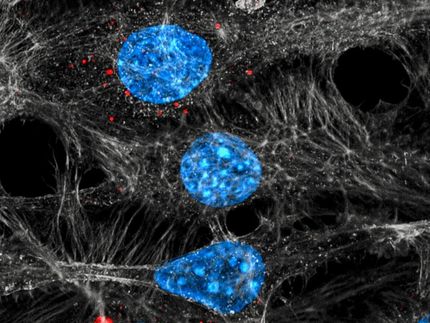
Critical to achieving those results were the size and surface structure of the nanotubes, which governed how they interacted with the walls of the blood vessels through which they circulated after being injected. Though a leaky vessel - nautical or anatomical - is rarely a good thing, in this instance the relatively leaky walls of blood vessels in the tumor tissue provided the opening that the nanotubes needed to slip into the tumor cells.
"The results are actually highly dependent on the surface chemistry," Dai said. "In other words, you don't get this result just by attaching drugs to any nanotubes."
The researchers used nanotubes that they had coated with polyethylene glycol (PEG), a common ingredient in cosmetics. The PEG they used was a form that has three little branches sprouting from a central trunk. Stuffing the trunks into the linked hexagonal rings that make up the nanotubes created a visual effect that Dai described as looking like rolled-up chicken wire with feathers sticking out all over. The homespun sounding appearance notwithstanding, the nanotubes proved to be highly effective delivery vehicles when the researchers attached the paclitaxel to the tips of the branches.