BGU researchers develop new fast test to tell bacterial and viral infections apart
Prof. Robert Marks and multi-disciplinary team tracked the immune system’s response to infection
Advertisement
Researchers at Ben-Gurion University of the Negev have developed a new type of test that would quickly and accurately distinguish between bacterial and viral infections. Currently tests take one to two days and aren’t always accurate enough for a clear-cut diagnosis. Meanwhile, patients continue to suffer from the symptoms untreated as they await test results. Moreover, treating a viral infection with antibiotics merely increases the body’s resistance to antibiotics.
A multi-disciplinary team, headed by Prof. Robert Marks, of the Department of Biotechnology Engineering and the National Institute for Biotechnology in the Negev (NIBN), made the discovery that will enable better diagnostics as well as the prevention of the misuse of prescribed antibiotics.
“A group at BGU has shown it is possible to distinguish a patient's infection as either viral or bacterial by merely studying the glow produced by a sample of their blood,” he said.
Team member and doctoral student Daria Prilutsky undertook the project as part of her Interdisciplinary Technologies Fellowship from the Planning and Budgeting Committee of the Council for Higher Education.
“We discovered that phagocytic cells, circulating in our body, inherit different pieces of information in different diseases and are ’pre-tuned for future tasks‘, therefore, they possess predictive value that can be used as a sensitive marker to distinguish between various clinical states,” Prilutsky added.
Writing in the American Chemistry Society’ Journal Analytical Chemistry, Prilutsky et al outlined the study they did of 69 patients admitted to Soroka University Medical Center in Beer-Sheva with various types of infections. Rather than looking at the infection, they looked at the immune system’s response to the infection.
“Upon activation of phagocytes, an increase in the consumption of molecular oxygen occurs, which results in the production of reactive oxygen species (ROS), a process collectively called respiratory burst. When luminol is added to the system, the ROS generation is accompanied by light emission (chemiluminescence, CL). Thus, CL is a sensitive marker of the oxidative potential of phagocytes, which can be recorded as a luminoldependent CL (LCL),” they wrote.
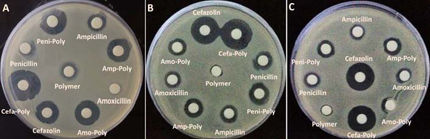
Their study clearly indicated that phagocytes react differently to viral and bacterial infections and that CL can distinguish those reactions. Using C4.5 decision tree data mining, the group was able to achieve 88.9% prediction accuracy in blind cases.
“The approach of inspecting whole-blood CL as a measure of respiratory burst, analysis of kinetics, and classification of clinical groups using data mining algorithms demonstrated a high predictive diagnostic value and may assist in proper treatment modalities a very short time after admission of the patient to the hospital,” they wrote.