Antibodies prevent cell infection
The findings are important for the development of new drugs against highly resistant infectious agents
Advertisement
Using bacteria of the Bartonella henselae species, researchers from Goethe University, Frankfurt University Hospital, the Paul Ehrlich Federal Institute for Vaccines and Biomedicines in Langen, and the University of Oslo demonstrated for the first time that antibodies can prevent certain surface proteins of bacterial pathogens from entering host cells. The findings are important for the development of new drugs against highly resistant infectious agents.
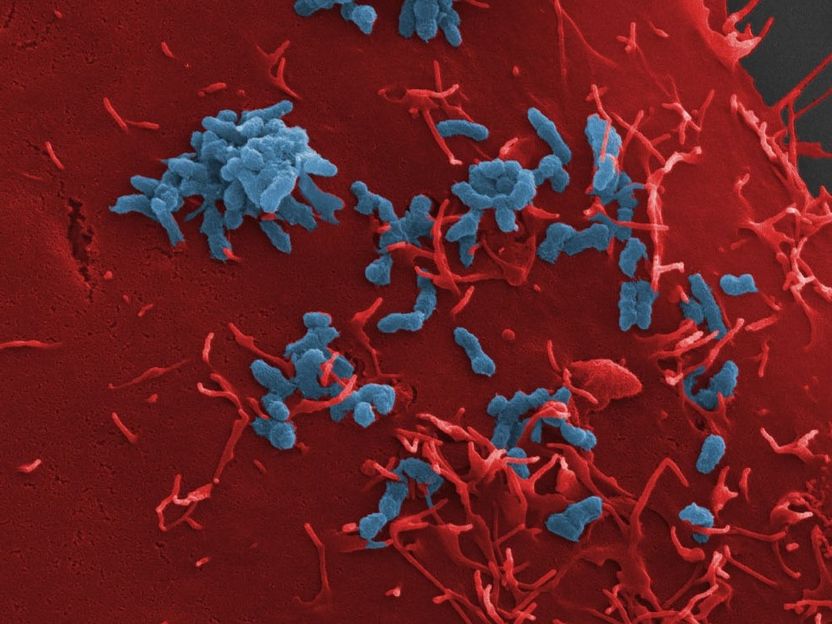
Adhesion of Bartonella henselae (blue) to human blood vessel cells (red). The bacterium's adhesion to the host cells could be blocked with the help of so-called “anti-ligands".
https://www.mdpi.com/2075-4418/11/7/1259
Infections, especially those with highly resistant pathogens, pose a significant threat to human health. It is dangerous when pathogens manage to colonize the organism and subsequently cause severe infections. The first step in such an infection always consists of the pathogens attaching themselves to the host cells’ surface. From here, the infections spread, resulting, for example, in infections of deeper tissue layers and organs.
A group of scientists surrounding Prof. Volkhard Kempf from Frankfurt University Hospital’s Institute of Microbiology and Hospital Hygiene has now succeeded in blocking this adhesion mechanism in a bacterium, thereby preventing the infection of host cells. For this purpose, the researchers examined the pathogen Bartonella henselae, usually causing cat scratch disease. Transmitted by cats, the disease mainly affects young children, whose symptoms include swollen and hardened lymph nodes around the site of infection – usually following a scratch or bite injury caused by infected cats.
Bartonella bacteria infect so-called endothelial cells, which line the blood vessels. Via their surface protein Bartonella adhesin A (BadA), they attach themselves to a protein (fibronectin) of the so-called "extracellular matrix", a network of protein fibers that lie on top of the endothelial cells.
To determine which parts of the BadA protein are important in the bacterial adhesion process, the researchers equipped Bartonella bacteria with various genetically modified BadA variants, among others, and then analyzed the extent to which these variants were still able to bind fibronectin. Once it was clear which BadA segments were responsible for the binding, the team produced antibodies against them, using cell culture experiments to show for the first time that such antibodies can prevent infection by such bacteria.
Prof. Volkhard Kempf explains: "Bartonella henselae is not a very dangerous pathogen, and in most cases, cat scratch disease does not require any specific medical treatment. However, for us Bartonella henselae is a very important model organism for far more dangerous pathogens such as Acinetobacter baumannii, a serious pathogen that usually causes wound infection or pneumonia and often shows resistance to several last-choice antibiotics. The BadA protein of Bartonella henselae belongs to the so-called 'trimeric autotransporter adhesins', which are also responsible for adhesion to human cells in Acinetobacter and a number of other pathogens. A drug-induced blocking of these adhesins is therefore a promising novel and future approach to combat dangerous bacterial infections."
Original publication
Other news from the department science
Most read news
More news from our other portals
See the theme worlds for related content
Topic world Antibodies
Antibodies are specialized molecules of our immune system that can specifically recognize and neutralize pathogens or foreign substances. Antibody research in biotech and pharma has recognized this natural defense potential and is working intensively to make it therapeutically useful. From monoclonal antibodies used against cancer or autoimmune diseases to antibody-drug conjugates that specifically transport drugs to disease cells - the possibilities are enormous
Topic world Antibodies
Antibodies are specialized molecules of our immune system that can specifically recognize and neutralize pathogens or foreign substances. Antibody research in biotech and pharma has recognized this natural defense potential and is working intensively to make it therapeutically useful. From monoclonal antibodies used against cancer or autoimmune diseases to antibody-drug conjugates that specifically transport drugs to disease cells - the possibilities are enormous