Unstoppable against blood cancer
What was previously only possible in the mouse model, the researchers now show in human cells
Advertisement
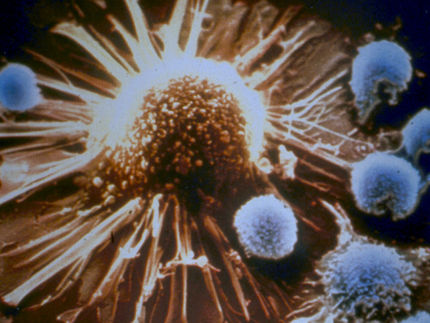
For people with certain forms of leukemia, lymphoma or multiple myeloma, they are sometimes the last chance to beat the cancer: Treatments with chimeric antigen receptor T cells, or CAR T cells for short. For this purpose, T cells are taken from the patient's blood to equip them with artificially produced receptors, or CARs, outside the body. As guardians of the immune system, T cells constantly patrol vessels and tissues to detect foreign structures. CARs also enable them to recognize specific surface structures on cancer cells. Given back to the patient via infusion, they then circulate in the body as a "living drug", binding highly specifically to tumor cells and destroying them.
The modified immune cells remain permanently in the organism, multiply and go into action again if the cancer flares up again - or so the theory goes. In practice, however, many patients still experience a relapse. This is because the tumor cells use a trick to slow down the CAR-T cells: they produce more of the protein EBAG9, but also stimulate its synthesis in the T cells. In the immune cells, EBAG9 inhibits the release of cell-toxic enzymes - in other words, slows down the desired immune response.
Already in June 2022, a team led by the last authors Dr. Armin Rehm and Dr. Uta Höpken from the Max Delbrück Center for Molecular Medicine in the Helmholtz Association (MDC) showed in the scientific journal "JCI Insight" that the immune response against cancer cells is permanently enhanced when they switch off the EBAG9 gene in mice. The rodents also developed more T memory cells. They are part of the immunological memory that increases its responsiveness after the first contact with a cancer antigen.
Now the researchers have been able to demonstrate these key findings in vitro in human CAR-T cells as well. The decisive step towards therapeutic application has thus been achieved, the team now reports in "Molecular Therapy". "In the absence of EBAG9, more radical tumor cell eradication occurs earlier, which presumably not only leads to longer-lasting therapeutic successes, but also opens up real chances of a cure," Rehm says.
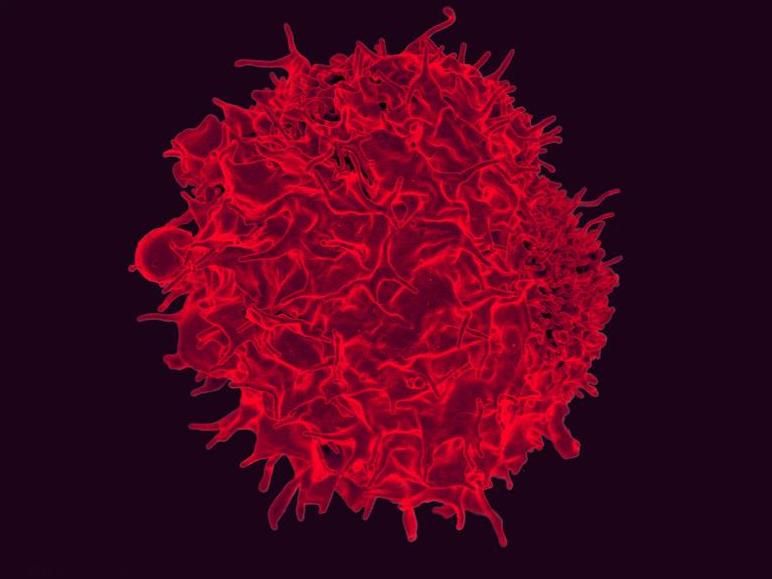
Stained scanning electron micrograph of a T lymphocyte.
NIAID, CC BY 2.0
Putting the brakes on immunotherapy
Even when the EBAG9 gene was discovered, scientists recognized that it played an important role in cancer. But exactly which role remained unclear for a long time. When the MDC team entered the field in 2009, they first noticed that mice lacking the gene coped much more easily with bacterial and viral infections than their peers and formed more memory T cells, which are of particular interest for tumor biology.
Then in 2015, first author Dr. Anthea Wirges successfully throttled the synthesis of the protein EBAG9 using microRNAs. For the current study, the researcher cultured "disinhibited" CAR-T cells in this way together with various human blood or lymph node cancer cells. Just as before in the mouse model, tumor growth was significantly reduced. Recurrences also developed much later.
"By releasing the EBAG9 brake, the genetically modified T cell can secrete more cytotoxic substances. However, it does not ignite a stronger cytokine storm, which is a typical side effect of CAR therapy," Wirges explains. On the contrary, the risk can even be minimized because fewer cells than usual need to be used. "Switching off the immune brake works universally. We can apply this to any CAR-T cell we make - no matter what form of blood cancer it targets."
The next step is clinical trials
However, the first therapy for blood cancer is and will remain chemotherapy, plus classic antibody therapy, because many patients* respond very well to it. "Only when the cancer returns does CAR therapy come into play. It is very expensive because it is an individual cellular product for only one person," says Höpken. One that can be used to save a life with a one-time treatment.
EBAG9 shows how important it is to persevere in research and have staying power. Wirges was spurred on by the fact that at the end of her work there is a real opportunity for clinical application. "Projects like this allow you to first learn techniques in basic research and then apply everything in translational research - right down to toxicological screening for regulatory processes," adds Rehm. The project has now reached this last point: In November, the researchers will present their concept to the Paul Ehrlich Institute, the German regulatory authority.
From animal models and in vitro experiments with human cells, the team now knows that the solubilized EBA9 brake is very effective, but does not lead to more side effects than conventional CAR-T cell therapy. "Now we need courageous clinicians and a partner to fund the clinical trials," Rehm says. If all goes well, unbraked CAR-T cell therapy could be available to patients as early as two years from now.
Note: This article has been translated using a computer system without human intervention. LUMITOS offers these automatic translations to present a wider range of current news. Since this article has been translated with automatic translation, it is possible that it contains errors in vocabulary, syntax or grammar. The original article in German can be found here.