To use all functions of this page, please activate cookies in your browser.
my.bionity.com
With an accout for my.bionity.com you can always see everything at a glance – and you can configure your own website and individual newsletter.
- My watch list
- My saved searches
- My saved topics
- My newsletter
Supraventricular tachycardia
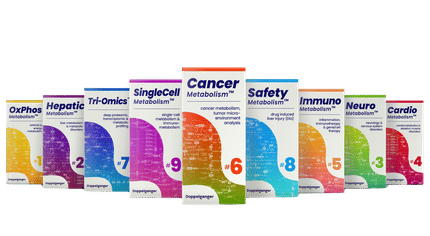
A supraventricular tachycardia (SVT) is a tachycardia or rapid rhythm of the heart in which the origin of the electrical signal is either the atria or the AV node. These rhythms, by definition, are either initiated or maintained by the atria or the AV node. This is in contrast to the deadlier ventricular tachycardias, which are rapid rhythms that originate from the ventricles of the heart, that is, below the atria or AV node. Product highlight
SymptomsSymptoms can come on suddenly and may go away without treatment. They can last a few minutes or as long as 1-2 days. The rapid beating of the heart during SVT can make the heart a less effective pump so that the cardiac output is decreased and the blood pressure drops. The following symptoms are typical with a rapid pulse of 140-250 beats per minute:
TerminologyThe term supraventricular tachycardia is often used differently in different settings. Properly, it refers to any tachycardia that is not ventricular in origin. This definition includes sinus tachycardia. Often, however, in a clinical setting, it is used loosely as a synonym for paroxysmal supraventricular tachycardia (PSVT), which refers to those SVTs that have a sudden, almost immediate onset. A person experiencing PSVT may see his heart rate go from 90 to 180 beats per minute instantaneously. Because sinus tachycardias (and some other SVTs) have a gradual (i.e. non-immediate) onset, they are excluded from the PSVT category. PSVTs are usually AV nodal reentrant tachycardias. Types of SVTsThe following are types of supraventricular tachycardias, each with a different mechanism of impulse maintenance: SVTs from a SINOATRIAL source:
SVTs from an ATRIAL source:
SVTs from an ATRIOVENTRICULAR source:
DiagnosisMost supraventricular tachycardias have a narrow QRS complex on EKG, but it is important to realise that supraventricular tachycardia with aberrant conduction (SVTAC) can produce a wide-complex tachycardia that may mimic ventricular tachycardia (VT). In the clinical setting, it is important to determine whether a wide-complex tachycardia is an SVT or a ventricular tachycardia, since they are treated differently. Ventricular tachycardia has to be treated appropriately, since it can quickly degenerate to ventricular fibrillation and death. A number of different algorithms have been devised to determine whether a wide complex tachycardia is supraventricular or ventricular in origin.[1] In general, a history of structural heart disease dramatically increases the likelihood that the tachycardia is ventricular in origin. The individual subtypes of SVT can be distinguished from each other by certain physiological and electrical characteristics, many of which present in the patient's EKG.
Acute TreatmentIn general, SVT is not life threatening, but episodes should be treated or prevented. While some treatment modalities can be applied to all SVTs with impunity, there are specific therapies available to cure some of the different sub-types. Cure requires intimate knowledge of how and where the arrhythmia is initiated and propagated. The SVTs can be separated into two groups, based on whether they involve the AV node for impulse maintenance or not. Those that involve the AV node can be terminated by slowing conduction through the AV node. Those that do not involve the AV node will not usually be stopped by AV nodal blocking manoevres. These manoevres are still useful however, as transient AV block will often unmask the underlying rhythm abnormality. AV nodal blocking can be achieved in at least three different ways: Physical manoeuvresA number of physical manoevres cause increased AV nodal block, principally through activation of the parasympathetic nervous system, conducted to the heart by the Vagus nerve. These manipulations are therefore collectively referred to as Vagal Manoevres. The best recognised of these is the Valsalva maneuver, which increases intra-thoracic pressure and affects baro-receptors (pressure sensors) within the arch of the aorta. This can be achieved by asking the patient to hold their breath and "bear down" as if straining to pass a bowel motion, or less embarrassingly, by getting them to hold their nose and blow out against it. Plunging the face into, or just drinking a glass of ice cold water is also often effective. Firmly pressing the bulb at the top of one of the carotid arteries in the neck (carotid sinus massage, stimulating carotid baro-receptors) is also effective, but not recommended for those without adequate medical training. Drug TreatmentAnother modality involves treatment with medications. Prehospital care providers and hospital clinicians might administer Adenosine, an ultra short acting AV nodal blocking agent. If this works, followup therapy with Diltiazem, Verapamil or Metoprolol may be indicated. SVT that does NOT involve the AV node may respond to other anti-arrhythmic drugs such as Sotalol or Amiodarone. In pregnancy, Metoprolol is the treatment of choice as recommended by the American Heart Association. Electrical CardioversionIf physical maneuvers or drugs do not work, or if the patient is extremely unstable, a DC shock delivered to the chest (synchronized cardioversion) may also be used, and is almost always effective. Prevention & CureOnce the acute episode has been terminated, ongoing treatment may be indicated to prevent a recurrence of the arrhythmia. Patients who have a single isolated episode, or infrequent and minimally symptomatic episodes usually do not warrant any treatment except observation. Patients who have more frequent or disabling symptoms from their episodes generally warrant some form of preventative therapy. A variety of drugs including simple AV nodal blocking agents like beta-blockers and verapamil, as well as anti-arrhythmics may be used, usually with good effect, although the risks of these therapies need to be weighed against the potential benefits. For supraventricular tachycardia caused by a re-entrant pathway, another form of treatment is radiofrequency ablation. This is a low risk procedure that uses a catheter inside the heart to deliver radiofrequency energy to locate and destroy the abnormal electrical pathways. Ablation has been shown to be highly effective: up to 99% effective in eliminating AVNRT, and similar results in typical Atrial Flutter. Notable casesAfter being successfully diagnosed and treated, Bobby Julich went on to place 3rd in the 1998 Tour de France and win a Bronze Medal in the 2004 Summer Olympics.[2] See also
References |
|||||||
| This article is licensed under the GNU Free Documentation License. It uses material from the Wikipedia article "Supraventricular_tachycardia". A list of authors is available in Wikipedia. |