Huntington's disease protein helps wire the young brain
Protein in neurodegenerative disease found to build neuronal circuits
The protein that is mutated in Huntington's disease is critical for wiring the brain in early life, according to a new Duke University study.
Spencer McKinstry
Huntington's disease is a progressive neurodegenerative disorder that causes a wide variety of symptoms, such as uncontrolled movements, inability to focus or remember, depression and aggression. By the time these symptoms appear, usually in middle age, the disease has already ravaged the brain.
The new findings, published in the Journal of Neuroscience, add to growing evidence that Huntington's and other neurodegenerative disorders, such as Alzheimer's disease, may take root during development, said lead author Cagla Eroglu, an assistant professor of cell biology in the Duke University Medical School, and member of the Duke Institute for Brain Sciences.
"The study is exciting because it means that, if we understand what these developmental errors are, we may be able to interfere with the first stage of the disease, before it shows itself," Eroglu said.
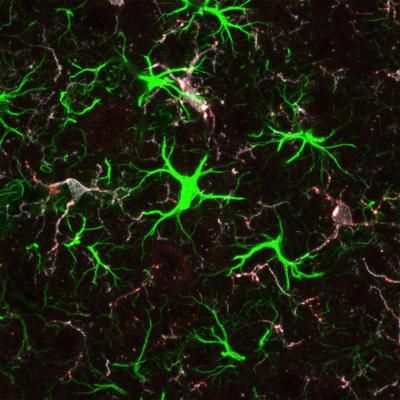
Several years ago, Eroglu and her team were looking for molecular players involved in the formation of new connections, or synapses, in early brain development in mice when their studies unexpectedly hit on the huntingtin (Htt) protein, which is present throughout the body and which forms clumps in the brain cells of people with Huntington's disease.
"(Htt) had been implicated in certain cellular functions and synaptic dysfunction in Huntington's, but the possibility that Htt is playing a direct role in synapse formation was not explored," Eroglu said.
To understand the protein's role as synapses form, the scientists created mice in which Htt is deleted only in the cortex, a part of the brain that is implicated in the disease and that controls perception, memory and thought.
At three weeks of age (roughly similar to the first two years of human life), a time when a mouse begins to take in its surroundings through its eyes and ears, the synapses of the mutant mice formed more rapidly compared with those of healthy mice, the scientists found.
But by five weeks, when some synapses typically strengthen while others weaken in a normal process called pruning, the synapses had completely deteriorated in the mutant mice. In collaboration with another Duke researcher, Henry Yin, an assistant professor in psychology & neuroscience, the team also investigated the changes in synaptic function in these mutant mice and found severe alterations of the synaptic physiology.
Not only did the researchers see faulty circuits in the mice missing cortical Htt, they also saw signs of cellular stress in the brain, in the exact spot within the cortex that projects to the striatum, another brain area targeted by Huntington's disease in people. "There's something about that particular circuit that is vulnerable to changes in Htt," Eroglu said.
The researchers also examined what happens in early brain development in a mouse model of Huntington's disease. Similar to people with the disease, these animals have one normal copy of the Htt gene, and one mutated copy, which produces a protein that is present in cells but in expanded form.
The researchers found the same pattern: the Huntington's disease model animals have synapses that initially mature much faster than normal in the cortex and then die off.
The new results also suggest that missing Htt for a prolonged period may not only affect the development but also the maintenance of healthy synapses, Eroglu said.
That's especially relevant to a current strategy for treating Huntington's disease: dialing down Htt levels in the brain using gene therapy or small-molecule inhibitors. But it has been a challenge to target the mutated copy of the gene, not the normal copy. Interested in the implications of lowering overall Htt levels, the group plans to delete Htt in the mouse brain later in life and measure the number of its synapses.
Other mouse models of the disease are also likely to have these faulty circuits. "We think this is probably a common thing, but that's something we're working on: whether we can detect early signs of faulty connections, correct it before the disease starts, and make these mice better," Eroglu said.