Biotechnology Breakthrough for Asthma
FDA approves Xolair, the first humanized antibody to target IgE, responsible for asthma with an allergic component
Advertisement
Genentech, Inc.Novartis Pharmaceuticals Corporation and Tanox, Inc. announced that the novel IgE-blocker Xolair® (Omalizumab) for subcutaneous use has been approved by the U.S. food and Drug Administration (FDA) for the treatment of moderate-to-severe persistent asthma in adults and adolescents. Xolair is the first humanized therapeutic antibody for the treatment of asthma and the first approved therapy designed to target the antibody IgE, a key underlying cause of the symptoms of asthma that has an allergic component. Xolair is expected to be available by prescription beginning July 2003.
Xolair is indicated for adults and adolescents (12 years of age and above) with moderate-to-severe persistent asthma who have a positive skin test or in vitro reactivity to a perennial aeroallergen and whose symptoms are inadequately controlled with inhaled corticosteroids. Xolair has been shown to decrease the incidence of asthma exacerbations in these patients. Safety and efficacy have not been established in other allergic conditions.
According to the National Institutes of Health, direct and indirect financial costs for all forms of asthma totaled $14 billion in 1998. In addition, asthma leads to at least two million emergency room visits and more than 5,000 deaths in the United States each year, according to the Center for Disease Control and Prevention's National Center for Health Statistics.
Xolair is being jointly developed under an agreement among Novartis Pharma AG, Genentech, Inc. and Tanox, Inc., and will be co-marketed in the United States by Genentech and Novartis Pharmaceuticals Corporation. In addition to approval in the United States, Xolair has also received marketing license from health authorities in Australia.
Clinical Study Results The companies' data submission to the FDA included two 52-week pivotal Phase III clinical trials with 1,071 asthma patients, 12 to 76 years of age, as well as data from several supportive safety and efficacy studies, including the 1,899-patient ALTO safety study. The pivotal trials were designed to study a reduction in asthma exacerbations. The co-primary endpoint of each study was the number of asthma exacerbations per patient during the stable-steroid phase and the steroid-reduction phase. Patients were randomized to receive subcutaneous Xolair or placebo every two or four weeks. Doses were determined based on patients' body weight and IgE level. Inhaled corticosteroid doses were kept stable over the initial 16 weeks of treatment (stable-steroid phase) and tapered during a further 12-week treatment period (steroid-reduction phase).
When used as an add-on therapy to inhaled corticosteroids, in both pivotal clinical trials, Xolair reduced mean asthma exacerbations ("asthma attacks") per patient by 33%-75% during the stable-steroid phase and 33%-50% during the steroid-reduction phase. Reduction in asthma exacerbations was confirmed by improvements in other measures of asthma control including symptom scores such as nocturnal awakenings and daytime asthma symptoms.
Safety Information Xolair has not been shown to alleviate asthma exacerbations acutely and should not be used for the treatment of acute bronchospasm or status asthmaticus. Systemic or inhaled corticosteriods should not be abruptly discontinued upon initiation of Xolair therapy. Decreases in corticosteroids should be performed only under the direct supervision of a physician and may need to be reduced gradually.
The most serious adverse reactions occurring in clinical studies with Xolair are malignancies (0.5% in Xolair vs. 0.2% in placebo) and anaphylaxis (<0.1% in Xolair). The difference in malignancy between the Xolair and placebo arms was not statistically significant. Xolair treatment is generally well tolerated. The most frequent adverse events included injection site reactions (45%), viral infections (23%), upper respiratory tract infections (20%), sinusitis (16%), headache (15%), and pharyngitis (11%). These events were observed at similar rates in Xolair-treated patients and control patients.
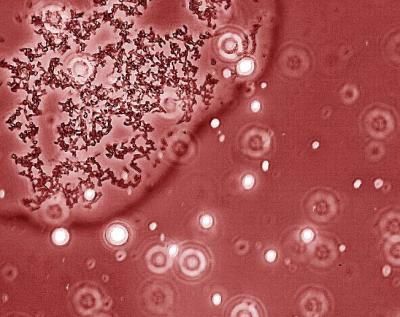
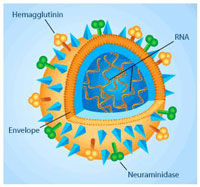
About IgE and the Allergic Cascade Asthma with an allergic component is a chronic inflammatory disorder of the airways, in which exposure to an aeroallergen triggers an allergic cascade that may result in airway inflammation and obstruction. In some patients, when allergens enter the body, IgE antibodies are produced and circulate in the blood. IgE circulating in the blood binds to mast cells, which contain the inflammatory chemicals (histamine, leukotrienes, others). Upon exposure to an allergen, IgE on the mast cell cross-links and triggers mast cells to release these chemicals. This chemical release triggers the inflammation, bronchial constriction and coughing associated with asthma. Xolair is designed to bind to the circulating IgE antibodies in the blood, decreasing the amount of IgE antibodies available to bind mast cells. With Xolair, fewer IgE antibodies can bind to mast cells, making IgE cross-linking on mast cells less likely and therefore inhibiting the mast cell's release of those chemicals that can lead to the symptoms of asthma.
Other news from the department research and development
Most read news
More news from our other portals
See the theme worlds for related content
Topic world Antibodies
Antibodies are specialized molecules of our immune system that can specifically recognize and neutralize pathogens or foreign substances. Antibody research in biotech and pharma has recognized this natural defense potential and is working intensively to make it therapeutically useful. From monoclonal antibodies used against cancer or autoimmune diseases to antibody-drug conjugates that specifically transport drugs to disease cells - the possibilities are enormous
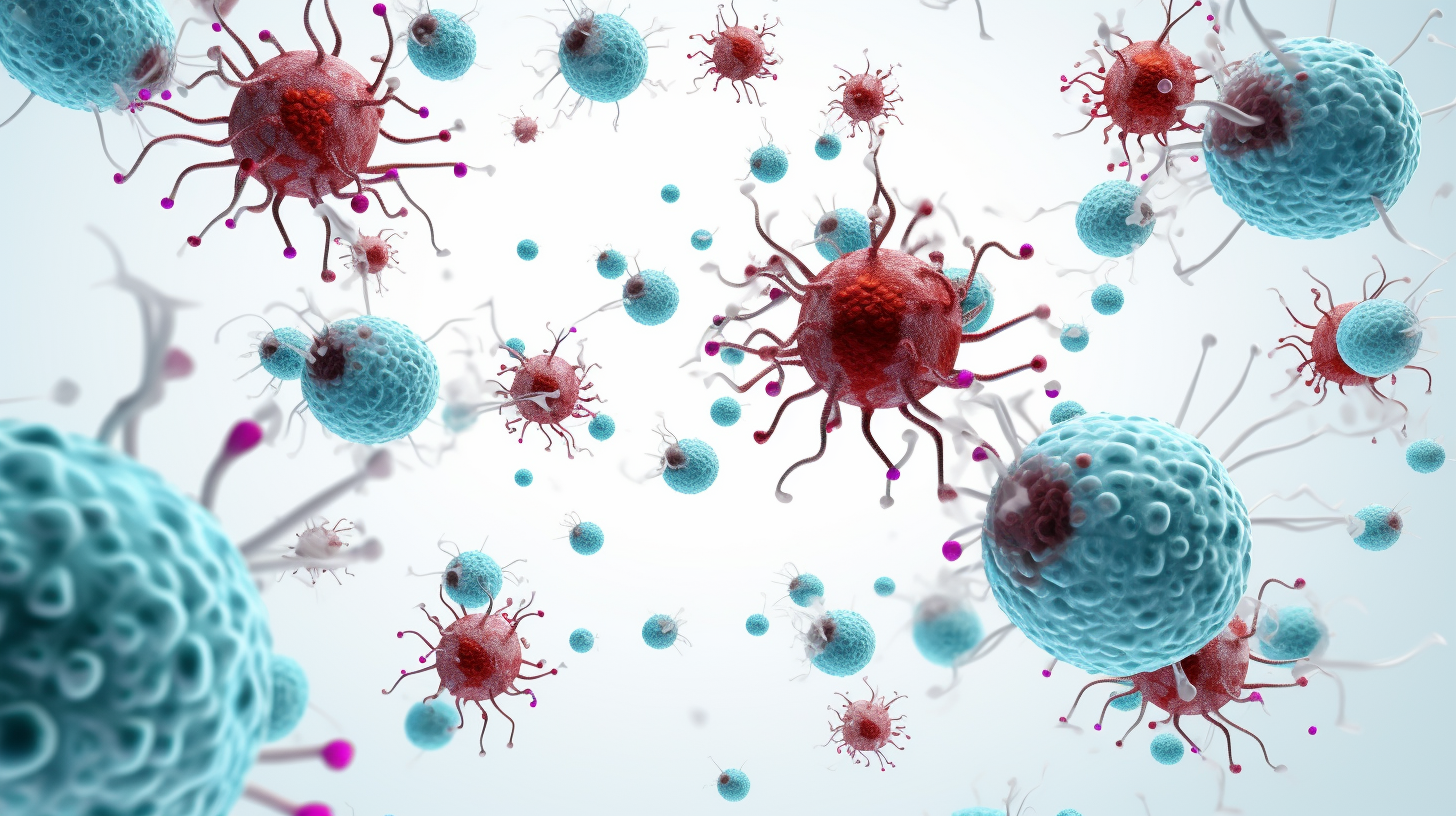
Topic world Antibodies
Antibodies are specialized molecules of our immune system that can specifically recognize and neutralize pathogens or foreign substances. Antibody research in biotech and pharma has recognized this natural defense potential and is working intensively to make it therapeutically useful. From monoclonal antibodies used against cancer or autoimmune diseases to antibody-drug conjugates that specifically transport drugs to disease cells - the possibilities are enormous