Killer cells: How the immune system selects its defense troops
Researchers investigate a fundamental biological process in vaccinated test subjects
Advertisement
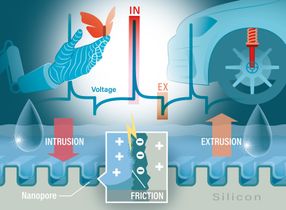
When killer cells of the immune system encounter signs of an infection, some of them divide rapidly. They grow into a large defense force that then fights the pathogen. However, this is by no means the case for every single killer cell. What is the criterion that determines whether they multiply or not? Researchers from Friedrich-Alexander-Universität Erlangen-Nürnberg (FAU), Erlangen University Hospital and Helmholtz Munich have investigated this question. They examined people who had received a Covid vaccination. In these people, only cells whose "potency" in relation to the vaccinated virus trait exceeded a certain threshold value divided. The results appear in the journal Science Immunology.
Pathogens can look very different. Nevertheless, the immune system is usually able to detect them quickly. It owes this ability in part to the approximately 100 million different types of cytotoxic T cells (also known as killer cells) that are on guard throughout the body. Each of them is trained to recognize foreign molecules - such as those from a potential invader. However, each of these types is on the lookout for a different warning signal: Some killer cells, for example, sound the alarm when they encounter a molecule from flu viruses. Others, on the other hand, may be activated by a specific tumor protein.
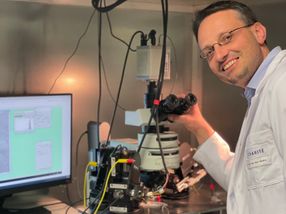
Sensors on the surface of the killer cells - the T-cell receptors - are responsible for this. They respond to very specific molecular recognition marks, which can look very different depending on the type of receptor. "We call these recognition marks antigens," explains Prof. Dr. Kilian Schober, Institute of Microbiology - Clinical Microbiology, Immunology and Hygiene (Director: Prof. Dr. Christian Bogdan) at Erlangen University Hospital. "T cell receptors can bind to antigens - but only if they fit them exactly, like a key to a lock."
"Clone warriors" of the immune system
When this happens, the killer cell can begin to divide rapidly. This creates a whole army of identical cells - a clone. They all have the same T-cell receptor as the mother cell and can therefore also recognize the corresponding antigen and fight the antigen-bearing cell. However, binding to a foreign molecule fragment does not always lead to a proliferation of the respective immune cell. "We wanted to know why this is the case," explains Schober. "To do this, we looked at the immune response of test subjects who had received a vaccination with an mRNA vaccine during the Covid pandemic."
mRNA vaccines cause body cells to produce a specific protein fragment of the coronavirus. This fragment is then detected by matching receptors and can thus activate the respective killer cells. In the event of a real infection, the body can then quickly fight the pathogen. As a rule, there are several hundred T cell receptors that can dock onto the virus protein. However, some of them are more precise than others - they therefore bind more strongly. In technical terms, they have a higher "avidity". "We have now been able to show that killer cells are only stimulated to divide if their avidity exceeds a certain threshold value," says Schober.
Diversity increases the effectiveness against mutants
Of the several hundred cell lines, this leaves a few dozen that each form a clone of defense cells. "However, it is not the case that the killer cells with the highest avidity multiply the most," emphasizes Schober's doctoral student Katharina Kocher, who carried out a large part of the experiments. "They have to have a certain minimum level of avidity in order to divide at all. However, the extent to which they do this and how large the respective clone of defense cells ultimately becomes seems to depend on chance." Shortly after vaccination, the immune system of the test subjects therefore formed around twenty to thirty killer cell clones of different sizes. Each of them had a different T-cell receptor, and yet all of them were able to bind sufficiently strongly to the virus protein formed after the vaccination.
This diversity of the defense troops is a great advantage, as the researchers were able to demonstrate experimentally: "If the virus mutates over time, this increases the likelihood that there are still killer cells that can fight it," explains Schober. "A single clone - however high its avidity - could never cover all possible mutants."
Such analyses from humans in particular are still rare. This also has to do with the enormous effort that the researchers had to put in: "We examined several thousand killer cells in each test subject and analyzed the structure of their receptors," says Schober. "We then recreated over a hundred individual receptors in a test system in order to measure their avidity." But the effort was worth it. "The results of our study provide an interesting insight into the strategies of the immune system, which may also benefit the development of new vaccines in the future."
Note: This article has been translated using a computer system without human intervention. LUMITOS offers these automatic translations to present a wider range of current news. Since this article has been translated with automatic translation, it is possible that it contains errors in vocabulary, syntax or grammar. The original article in German can be found here.
Original publication
Katharina Kocher, Felix Drost, Abel Mekonnen Tesfaye, Carolin Moosmann, Christine Schülein, Myriam Grotz, Elvira D’Ippolito, Frederik Graw, Bernd Spriewald, Dirk H. Busch, Christian Bogdan, Matthias Tenbusch, Benjamin Schubert, Kilian Schober; "Vaccination-induced T cell responses maintain polyclonality with high antigen receptor avidity"; Science Immunology, Volume 10