UK approves world's first therapy with gene scissors
Developers of the Crispr method were awarded the Nobel Prize in 2020: a drug using the gene scissors has now been approved for the first time
Advertisement
(dpa) In the UK, a drug based on the gene-scissor technology CRISPR has been approved for the first time worldwide. This was announced by the Medicines and Healthcare products Regulatory Agency (MHRA) on Thursday.
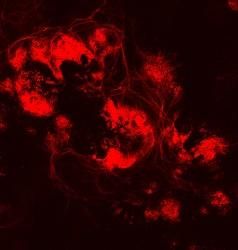
The drug, called "Casgevy", has been approved for the treatment of sickle cell disease and beta thalassemia in patients aged twelve and over. Both genetic blood disorders are caused by errors in the gene for haemoglobin. This is an iron-containing protein complex that is found in red blood cells and is used to transport oxygen.
The so-called Crispr/Cas gene scissors can be used to target individual genes. The developers of the method, Emmanuelle Charpentier and Jennifer A. Doudna, were awarded the Nobel Prize for it in 2020. "Casgevy" is used to modify the defective genes in patients' bone marrow stem cells so that they can produce functioning haemoglobin, according to a statement from the MHRA. To do this, stem cells are removed from the bone marrow, processed in the laboratory and then reintroduced into the patient. The therapy requires a hospital stay of several weeks. However, the result has the potential to have a lifelong effect, the report continued.
Both sickle cell disease and beta thalassemia are painful, lifelong conditions that could be fatal in some cases, said Julian Beach, interim executive director of the MHRA's Healthcare Quality and Access division. He added: "Until now, a bone marrow transplant - which must come from a well-matched donor and carries the risk of rejection - has been the only permanent treatment option."
Sickle cell disease can lead to severe bouts of pain, serious and life-threatening infections and anemia, also known as anemia, a lack of oxygen in the blood. Patients with beta-thalassemia also suffer from anemia and often require blood transfusions every three to five weeks.
Of 28 patients with sickle cell disease who were treated with the drug in a clinical trial, 97 percent were reportedly free of severe pain attacks for at least one year. In the clinical trial with beta-thalassemia patients who are dependent on blood transfusions, 93 percent (39 of 42 patients) did not need a transfusion of red blood cells for at least twelve months. In the remaining three patients, at least a 70 percent reduction
in blood transfusions was possible.
The drug is produced in a collaboration between the companies Vertex and CRISPR Therapeutics, which have their headquarters in the USA and Switzerland. According to a statement from the two companies, around 2,000 people in the UK are currently eligible for treatment with "Casgevy". Vertex Managing Director Reshma Kewalramani spoke of a "historic day in science and medicine". He hopes that this is just the first of many applications of the method that could benefit people with serious diseases, said CRISPR Therapeutics CEO Samarth Kulkarni, according to the press release.
Selim Corbacioglu from the University Hospital Regensburg, who has already tested a Crispr therapy himself, cites some concerns. "We cannot be 100 percent sure that the gene scissors will not alter other DNA segments," he said. "Crispr therapy is also not something that can be carried out 'just like that'." There are considerable side effects and the therapy is also very expensive.
According to Joachim Kunz from Heidelberg University Hospital, the therapy is "extremely complex, requires complex logistics and will foreseeably not be scalable indefinitely due to the resources required, but will only be available for a limited number of patients per year". Although the current clinical studies on Crispr therapy are promising, even the patients treated first have only been followed up for around four years. "Even if there is no evidence of this so far, it could be that the effect of gene therapy diminishes over the years because, for example, the lifespan of the manipulated blood stem cells is shortened."
Note: This article has been translated using a computer system without human intervention. LUMITOS offers these automatic translations to present a wider range of current news. Since this article has been translated with automatic translation, it is possible that it contains errors in vocabulary, syntax or grammar. The original article in German can be found here.