Scientists find way to make leukemia cells kill each other
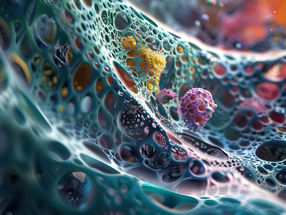
Scientists at The Scripps Research Institute (TSRI) have found a way to change leukemia cells into leukemia-killing immune cells. The surprise finding could lead to a powerful new therapy for leukemia and possibly other cancers.
"It's a totally new approach to cancer, and we're working to test it in human patients as soon as possible," said senior investigator Richard A. Lerner, Institute Professor and the Lita Annenberg Hazen Professor of Immunochemistry at TSRI.
The findings, published this week in the Proceedings of the National Academy of Sciences, result from the discovery of a rare human antibody.
Unexpected Effects
Recently, the lab mounted an effort to find therapies for people with certain immune cell or blood factor deficiencies, by looking for antibodies that activate growth-factor receptors on immature bone marrow cells that might induce these bone marrow cells to mature into specific blood cell types. Over the past few years, Lerner and his team succeeded in identifying a number of antibodies that activate marrow-cell receptors in this way.
In the process, the scientists noted that some of these receptor-activating antibodies have unexpected effects on marrow cells, causing them to mature into radically different cell types, such as neural cells.
While why this happens is an unresolved issue, the discovery led the team to wonder if they could also use the method to convert cancerous marrow cells into non-cancerous cells.
Following the Trail
To find out, in the new study Lerner and his team, including first author Kyungmoo Yea, an assistant professor of cellular and molecular biology at TSRI, tested 20 of their recently discovered receptor-activating antibodies against acute myeloid leukemia cells from human patients. One of these antibodies turned out to have an extraordinary impact on the acute myeloid leukemia cells.
A high percentage of acute myeloid leukemia cells express the thrombopoietin (TPO) receptor, and the effective antibody was a highly potent and selective activator of this receptor on marrow cells. When the antibody was applied to healthy immature marrow cells, it caused them to mature into blood-platelet-producing cells called megakaryocytes. However, when the antibody was applied to acute myeloid leukemia cells, they matured into very different cells known as dendritic cells, key support cells in the immune system.
By itself, this could be a valuable therapeutic strategy, but it wasn't the end of the story. Lerner's team noted that, with longer exposures to the antibodies and certain other lab-dish conditions, the induced dendritic cells developed further--into cells that closely resembled natural killer (NK) cells.
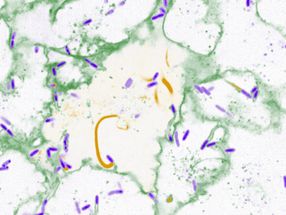
NK cells represent one of the rapid-reaction forces of the immune system. They can be effective against viruses and bacteria--and cancer cells--even without prior exposure. They don't have highly specific receptors for recognizing individual targets, as T-cells do, but instead are capable of detecting, in a general way, when a nearby cell is infected or cancerous.
"That antibody could have turned those acute myeloid leukemia cells into a lot of other cell types, but somehow we were lucky enough to get NK cells," Lerner said.
'Fratricide'
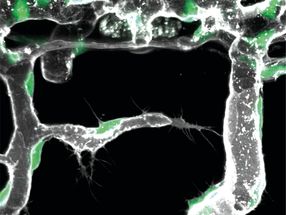
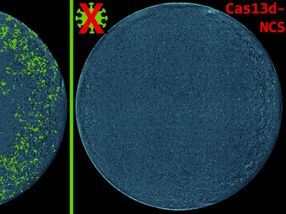
The team examined these induced NK cells with electron microscopy and observed that many of the cells had extended tendrils through the outer membranes of neighboring leukemic cells--their erstwhile brethren. In lab dish tests, a modest number of these NK cells wiped out about 15 percent of the surrounding acute myeloid leukemia cell population in just 24 hours.
Curiously, the induced NK cells' cancer-killing effect appeared to be purely fratricidal. The researchers found that unrelated breast cancer cells did not die off in large numbers when in the presence of the NK cells.
Why the induced NK cells appear to target only closely related cells isn't yet clear. In principle, though, there are yet-to-be-discovered antibodies--and even small-molecule compounds--that would turn other cancerous cell types into fratricidal NK cells, by activating other receptors expressed on those cells.
Such fratricidal therapies, which Lerner terms "fratricidins," would have several potential advantages. First, especially if they are antibodies, they could be clinically useful with little or no further modification. Second, their high specificity for their target receptors, and the resulting NK cells' specificity for related cancer cells, should reduce the likelihood of adverse side effects, possibly making them much more tolerable than traditional cancer chemotherapies.
Other news from the department science
Most read news
More news from our other portals
See the theme worlds for related content
Topic world Antibodies
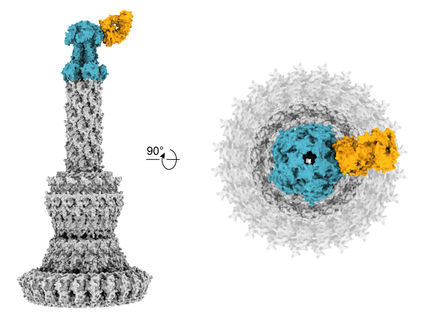
Antibodies are specialized molecules of our immune system that can specifically recognize and neutralize pathogens or foreign substances. Antibody research in biotech and pharma has recognized this natural defense potential and is working intensively to make it therapeutically useful. From monoclonal antibodies used against cancer or autoimmune diseases to antibody-drug conjugates that specifically transport drugs to disease cells - the possibilities are enormous
Topic world Antibodies
Antibodies are specialized molecules of our immune system that can specifically recognize and neutralize pathogens or foreign substances. Antibody research in biotech and pharma has recognized this natural defense potential and is working intensively to make it therapeutically useful. From monoclonal antibodies used against cancer or autoimmune diseases to antibody-drug conjugates that specifically transport drugs to disease cells - the possibilities are enormous