Removing programming material after inducing stem cells could improve their regeneration ability
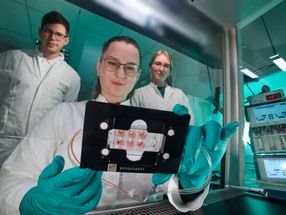
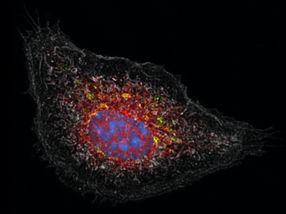
Human induced pluripotent stem cells (hiPSCs) have great potential in the field of regenerative medicine because they can be coaxed to turn into specific cells; however, the new cells don’t always act as anticipated. They sometimes mutate, develop into tumors or produce other negative side effects. But in a new study recently published in STEM CELLS Translational Medicine, researchers appear to have found a way around this, simply by removing the material used to reprogram the stem cell after they have differentiated into the desired cells.
The study, by Ken Igawa, M.D., Ph.D., and his colleagues at Tokyo Medical and Dental University along with a team from Osaka University, could have significant implications both in the clinic and in the lab.
Scientists induce (differentiate) the stem cells to become the desired cells, such as those that make up heart muscle, in the laboratory using a “reprogramming transgene” – that is, a gene taken from one organism and introduced into another using artificial techniques.
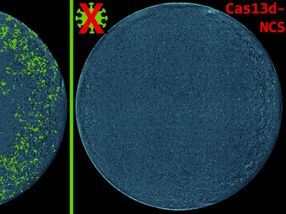
“We generated hiPSC lines from normal human skin cells using reprogramming transgenes, then we removed the reprogramming material. When we compared the transgene-free cells with those that had residual transgenes, both appeared quite similar,” Dr. Igawa explained. “However, after the cells’ differentiation into skin cells, clear differences were observed.”
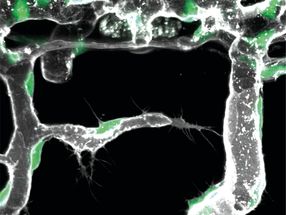
Several types of analyses revealed that the keratinocytes – cells that make up 90 percent of the outermost skin layer – that emerged from the transgene-free hiPSC lines were more like normal human cells than those coming from the hiPSCs that still contained some reprogramming material.
“These results suggest that transgene-free hiPSC lines should be chosen for therapeutic purposes,” Dr. Igawa concluded.
“Human induced pluripotent stem cell (hiPSC) lines have potential for therapeutics because of the customized cells and organs that can potentially be induced from such cells,” Anthony Atala, M.D., editor of STEM CELLS Translational Medicine and director of the Wake Forest Institute for Regenerative Medicine. “This study illustrates a potentially powerful approach for creating hiPSCs for clinical use.”
Original publication
Other news from the department science

Get the life science industry in your inbox
From now on, don't miss a thing: Our newsletter for biotechnology, pharma and life sciences brings you up to date every Tuesday and Thursday. The latest industry news, product highlights and innovations - compact and easy to understand in your inbox. Researched by us so you don't have to.